Kerala Plus One Zoology Notes Chapter 8 Excretory Products and their Elimination
What is excretion?
Excretion is the elimination common nitrogenous wastes. Ammonia, urea and uric acid are the major forms of nitrogenous wastes excreted by the animals.
Ammonotelic, ureotelic and urecotelic animals and their excretion:
1. The process of excreting ammonia is Ammonotelism. eg: Many bony fishes, aquatic amphibians and aquatic insects are ammonotelic.
2. Mammals, many terrestrial amphibians and marine fishes mainly excrete urea and are called ureotelic animals.
3. Reptiles, birds, land snails and insects excrete nitrogenous wastes as uric acid in the form of pellet or paste with a minimum loss of water and are called uricotelic animals.
Where is urea produced?
Ammonia produced by metabolism is converted into urea in the liver and released into the blood which is filtered and excreted out by the kidneys.
Excretion in lower organisms:
| Protonephridia or flame cells are the excretory structures in Platyhelminthes (Flatworms, eg: Planaria), rotifers, some annelids and the cephalochordate – Amphioxus. Nephridia are the tubular excretory structures of earthworms and other annelids Malpighian tubules are the excretory structures of most of the insects including cockroaches. Antennal glands or green glands perform the excretory function in crustaceans like prawns. |
Human Excretory System
In humans, the excretory system consists of
- A pair of kidneys
- One pair of ureters
- A urinary bladder
- A urethra.
Each kidney of an adult human measures 10 – 12 cm in length, 5 – 7 cm in width, 2 – 3 cm in thickness with an average weight of 120 – 170 g.
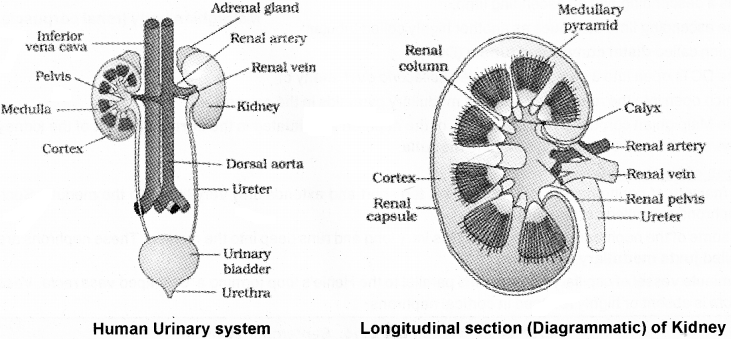
1. Centre of the inner concave surface of the kidney is a notch called hilum through which ureter, blood vessels and nerves enter.
2. Innerto the hilum is a broad funnel shaped space called the renal pelvis with projections called calyces.
3. Inside the kidney, there are two zones, an outer cortex and an inner medulla.
4. The medulla is divided medullary pyramids projecting into the calyces.
5. The cortex extends in between the medullary pyramids as renal columns called Columns of Bertini.
6. Each kidney has nearly one million complex tubular structures called nephrons, which are the functional units. A diagrammatic representation of a nephron showing blood vessels, duct and tubule Each nephron has two parts -1 The glomerulus & 2 Renal tubule.
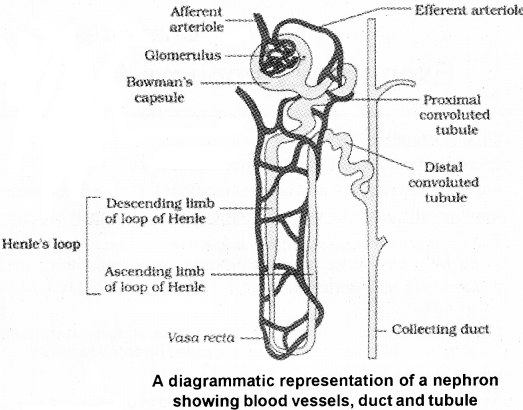
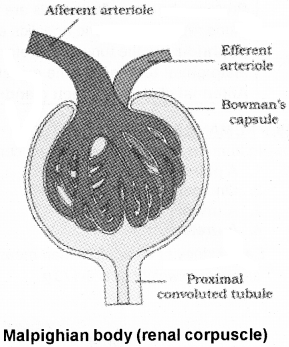
7. Glomerulus is a tuft of capillaries formed by the afferent arteriole – a fine branch of renal artery.
8. Blood from the glomerulus is carried away by an efferent arteriole.
9. The renal tubule begins with a double walled cup-like structure calle Bowman’s capsule, which encloses the glomerulus.
10. Glomerulus alongwith Bowman’s capsule, is called the malpighian body or renal corpuscle
11. The tubule continues further to form a highly coiled network proximal convoluted tubule (PCT).
12. A hairpin-shaped Henle’s loop is the next part of the tubule which has a descending and an ascending limb.
13. The ascending limb continues as another highly coiled tubular region called distal convoluted tubule (DCT).
14. The DCTs open into a straight tube called collecting duct, many of which open into the renal pelvis through medullary pyramids in the calyces.
15. The Malpighian corpuscle, PCT and DCT of the nephron are situated in the cortical region of the kidney whereas the loop of Henle dips into the medulla.
Types of Nephrons:
1. In majority of nephrons, the loop of Henle is too short and extends only very little into the medulla. Such nephrons are called cortical nephrons.
2. In some of the nephrons, the loop of Henle is very long and runs deep into the medulla.These nephrons are called juxta medullary nephrons. A minute vessel of capillary network runs parallel to the Henle’s loop forming a ‘LT shaped vasa recta. Vasa recta is absent or highly reduced in cortical nephrons.
Urine Formation
1. It involves three main processes namely, glomerular filtration, reabsorption and secretion
2. The first step in urine formation is the filtration of blood, which is carried out by the glomerulus and is called glomerular filtration.
3. 1100 – 1200 ml of blood is filtered by the kidneys per minute. The glomerular capillary blood pressure causes filtration of blood through 3 layers,
| (a) Endothelium of glomerular blood vessels (b) Epithelium of Bowman’s capsule and (c) Basement membrane between these two layers. |
4. The epithelial cells of Bowman’s capsule called podocytes which possess minute spaces called filtration slits.
5. Blood is filtered through these membranes, that almost all the constituents of the plasma except the proteins pass onto the lumen of the Bowman’s capsule. It is the process of ultrafiltration.
| Glomerular filtration in a healthy individual is approximately 125 ml/minute, i.e., 180 litres per day |
6. The kidneys have an efficient mechanism for the regulation of glomerular filtration rate. It is carried out by the juxtaglomerular apparatus (JGA).JGA is found in the distal convoluted tubule.
7. A fall in GFR can activate the JG cells to release renin which can stimulate the glomerular blood flow and thereby the GFR back to normal.
8. Nearly 99 percent of the filtrate is reabsorbed by the renal tubules. This process is called reabsorption.
9. For example, substances like glucose, amino acids, Na+, etc., in the filtrate are reabsorbed actively whereas the nitrogenous wastes and water are absorbed by passive transport.
10. During urine formation, the tubular cells secrete substances like H+, K+ and ammonia into the filtrate.
11. Tubular secretion is helpful in the maintenance of ionic and acid-base balance of body fluids.
Function Of The Tubules
Proximal Convoluted Ttubule (PCT):
1. PCT consists of simple cuboidal brush border epithelium which increases the surface area for reabsorption.
2. All essential nutrients, and 70 – 80 percent of electrolytes and water are reabsorbed by this segment.
3. PCT also helps to maintain the pH and ionic balance of the body fluids. It occurs through selective secretion of hydrogen ions, ammonia and potassium ions into the filtrate and by absorption of HCO3– from it.
Henle’s Loop
Function:
It helps to maintain high osmolarity of medullary interstitial fluid. The descending limb of loop of Henle is permeable to water but impermeable to electrolytes. This concentrates the filtrate as it moves down.
The ascending limb is impermeable to water but allows transport of electrolytes actively or passively. Therefore, as the concentrated filtrate pass upward, it gets diluted due to the passage of electrolytes to the medullary fluid.
Distal Convoluted Tubule (DCT):
The reabsorption of Na+, HCO3– and water takes place in this segment. In this segment selective secretion of hydrogen and potassium ions and NH3 to maintain the pH and sodium-potassium balance in blood.
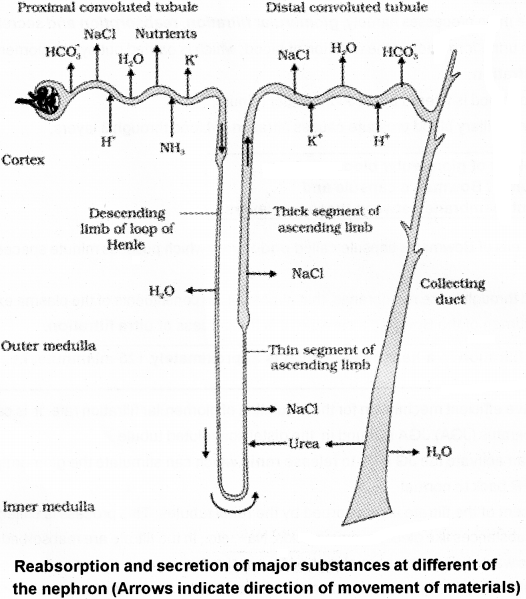
Collecting Duct:
It extends from the cortex of the kidney to the inner parts of the medulla. Large amounts of water is reabsorbed from this region to produce concentrated urine. This part maintains pH and ionic balance of blood by the selective secretion of H+ and K+ ions.
Mechanism Of Concentration Of The Filtrate
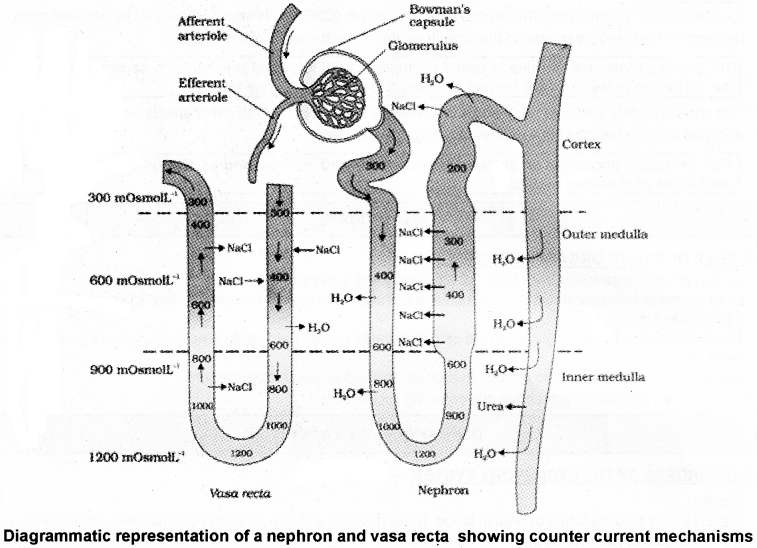
The flow of filtrate in the two limbs of Henle’s loop is in opposite directions and thus forms a counter current. The flow of blood through the two limbs of vasa recta is also in a counter current pattern.
The proximity between the Henle’s loop and vasa recta, as well as the counter current in them help in maintaining an increasing osmolarity towards the inner medullary interstitium, i.e. from 300 mOsmolL-1 in the cortex to about 1200 mOsmolL-1 in the inner medulla. This gradient is mainly caused by NaCl and urea.
NaCl is transported by the ascending limb of Henle’s loop which is exchanged with the descending limb of vasa recta. NaCl is returned to the interstitium by the ascending portion of vasa recta. Similarly, small amounts of urea enterthe thin segment of the ascending limb of Henle’s loop which is transported back to the interstitium by the collecting tubule.
This transport is facilitated by the counter current mechanism This mechanism helps to maintain a concentration gradient in the medullary interstitium. Presence of such interstitial gradient helps in an easy passage of water from the collecting tubule thereby concentrating the filtrate (urine).
Regulation Of Kidney Function
The functioning of the kidneys is influenced by hypothalamus, JGA and to a certain extent, the heart in the body are activated by changes in blood volume.
How can diuresis is prevented in body?
The decrease of fluid from the body can activate these Osmoreceptors which stimulate the hypothalamus to release antidiuretic hormone (ADH) or vasopressin from the neurohypophysis. ADH facilitates water reabsorption Hence it prevents diuresis.
An increase in body fluid volume switch off the osmoreceptors and suppress the ADH release. ADH can also affect the kidney function by its constrictory effects on blood vessels. This causes an increase in blood pressure. An increase in blood pressure increase the glomerular blood flow and the GFR.
| A fall in glomerular blood flow/glomerular blood pressure/GFR can activate the JG cells to release renin which converts angiotensinogen in blood to angiotensin I and further to angiotensin II. Angiotensin II, increases the glomerular blood pressure and thereby GFR. Angiotensin II also activates the adrenal cortex to release Aldosterone. Aldosterone causes reabsorption of Na+ and water from the distal parts of the tubule. This also leads to an increase in blood pressure and GFR. This is known as the Renin-Angiotensin mechanism. |
| An increase in blood flow to the atria of the heart can cause the release of Atrial Natriuretic Factor (ANF). ANF can cause vasodilation (dilation of blood vessels) and thereby decrease the blood pressure. ANF mechanism acts as a check on the renin-angiotensin mechanism. |
Micturition
It is the voluntary signal from the central nervous system (CNS). This signal is initiated by the stretching of the urinary bladder in response to the stretch receptors on the walls of the bladder.
| The process of release of urine is called micturition and the neural mechanisms causing it is called the micturition reflex. An adult human excretes 1 to 1.5 litres of urine per day. |
The urine is slightly acidic (pH – 6.0) and has a characterestic odour. 25 – 30 gm of urea is excreted out per day. Analysis of urine helps to know malfunctioning of the kidney.
| For example, presence of glucose (Glycosuria) and ketone bodies (Ketonuria) in urine are indicative of diabetes mellitus. |
Role Of Other Organs In Excretion
Lungs remove large amounts of CO2 (18 litres/day) and water every day. Liver secretes bile-containing substances like bilirubin, biliverdin, cholesterol, degraded steroid hormones, vitamins and drugs.
The sweat and sebaceous glands in the skin eliminates watery fluid containing NaCl, small amounts of urea, lactic acid, etc. Sebaceous glands eliminates sterols, hydrocarbons and waxes through sebum. This secretion provides a protective oily covering for the skin.
Disorders Of The Excretory System
Uemia:
It leads to the accumulation of urea in blood. It lead to kidney failure. In such patients, urea can be removed by a process called hemodialysis.
Procedure of Dialysis:
Blood drained from a artery is pumped into a dialysing unit after adding an anticoagulant like heparin.The unit contains a coiled cellophane tube surrounded by a fluid (dialysing fluid).
The porous cellophane membrance allows the passage of molecules based on concentration gradient.
As nitrogenous wastes are absent in the dialysing fluid, the cleared blood is pumped back to the body through a vein after adding anti-heparin to it.
Remedy for kidney damage:
Kidney transplantation is the ultimate method in the correction of acute renal failures (kidney failure). A functioning kidney is used in transplantation from a donor to minimise its chances of rejection by the immune system of the host.
Renal calculi:
Stone or insoluble mass of crystallised salts (oxalates, etc.) formed within the kidney.
Glomerulonephritis:
Inflammation of glomeruli of kidney
NCERT SUPPLEMENTARY SYLLABUS
Diabetes Insipidus:
Antidiuretic hormone (ADH) is released from the posterior pituitary, prevents dehydration. It helps in the reabsorption of water by the distal parts of the kidney tubules and prevents diuresis. Deficiency of ADH leads to diabetes insipedus, that means huge amounts of dilute urine is formed followed by intense thirst.
The name itself (diabetes = overflow; insipidus = tasteless) distinguishes it from diabetes .mellitus (mel = honey), in which insulin deficiency causes large amounts of blood sugar to be lost in the urine
Artificial kidney:
Hemodialysis machine is known as an artificial kidney. Hemodialysis is an artificial process of removing toxic substances from the blood in patients of kidney failure.
